Under the severe situation of the global COVID-19 epidemic, more and more mutant strains have shown up and dominated some areas. The mutation of the virus is essentially a change in the genome, and the source of the mutation of COVID-19 is the “error” in the replication and amplification of the virus. As COVID-19 continues to spread among the population, every replication and proliferation inevitably brings the risk of mutation.
Variants worthy of attention and discussion often have several characteristics: increased transmission capacity, increased risk of secondary infection due to immune escape or decreased effectiveness of vaccines, decreased effectiveness of existing treatment drugs, and a certain position in the epidemic, that is, more cases of infection.
At present, 4 new variants have the greatest threat to humans, namely Alpha, Beta, Gamma, and Delta variants.
Alpha: once the mainstream variant
Scientists first measured the genome sequence of the Alpha variant in November 2020, and the sample used was from September, so the Alpha variant is likely to expand between the summer and autumn of 2020.
The most important feature of the Alpha variant is its strong transmission power. A study published in AAAS Public Health Emergency Collection shows that the transmission speed of the Alpha variant is 40-80% higher than that of the original virus strain. According to the Weekly Epidemiological and Operational updates from the WHO as of 26 July, Alpha variant has been found in 178 countries and regions around the world.
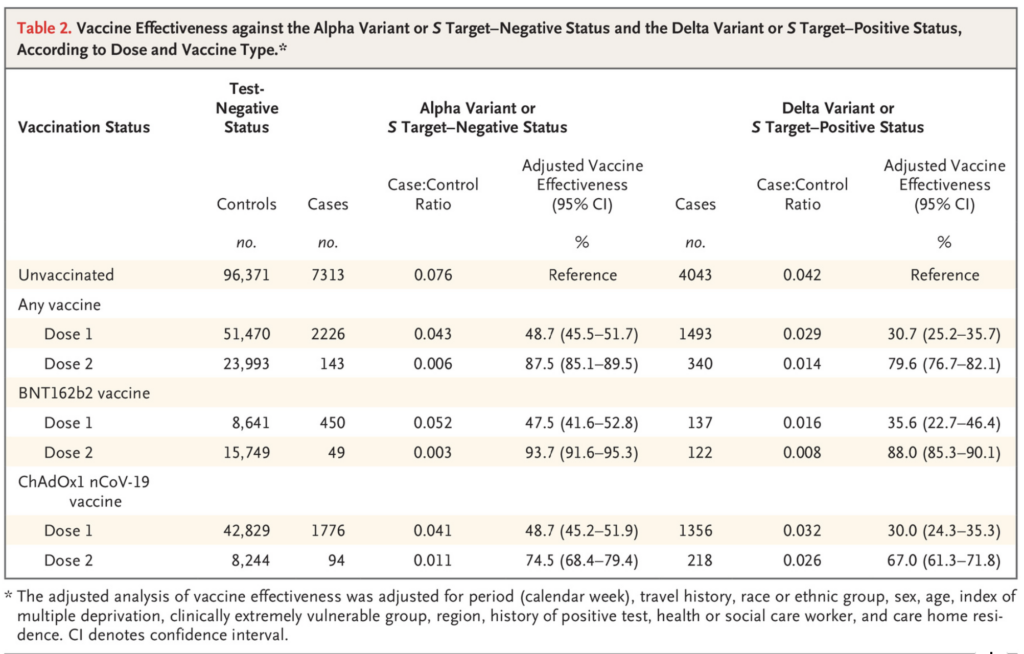
Although the spread is fast, fortunately Alpha does not significantly affect the effectiveness of the vaccine. For example, the Public Health England recently published a vaccine effectiveness tracking report in the New England Journal of Medicine. After receiving two doses of Pfizer/BioNTech vaccine, the effectiveness of protecting against Alpha variant against symptomatic COVID-19 was 93.7%, while the the effectiveness of the AstraZeneca vaccine is 74.5%, which is very consistent with the effectiveness data obtained in Phase III clinical trial of the vaccine and there was no Alpha variant at that time.
Beta: the most severe variant of immune escape
In the samples collected in South Africa in May 2020, scientists discovered the Beta variant and it soon became the main virus strain in South Africa. Beta variant has been recorded in 123 countries and regions around the world, according to the WHO.
But unlike Alpha variant’s dominant position in many countries, Beta variant has not shown a leading trend in the proportion of infection cases in most countries and regions. For example, the Beta variant detected in the United Kingdom and the United States accounted for 1% or even lower of infection case level.
The Beta variant has the highest degree of immune escape among known mutations. The immune escape of the coronavirus mutant strain has two major features in reality. One is that the human immunity obtained during the previous infection with the original virus strain is no longer reliable against the mutant strain, and the risk of secondary infection appears; the other is that the current vaccines are all based on the original virus strain design, and immune escape will threaten the effectiveness of the vaccine.
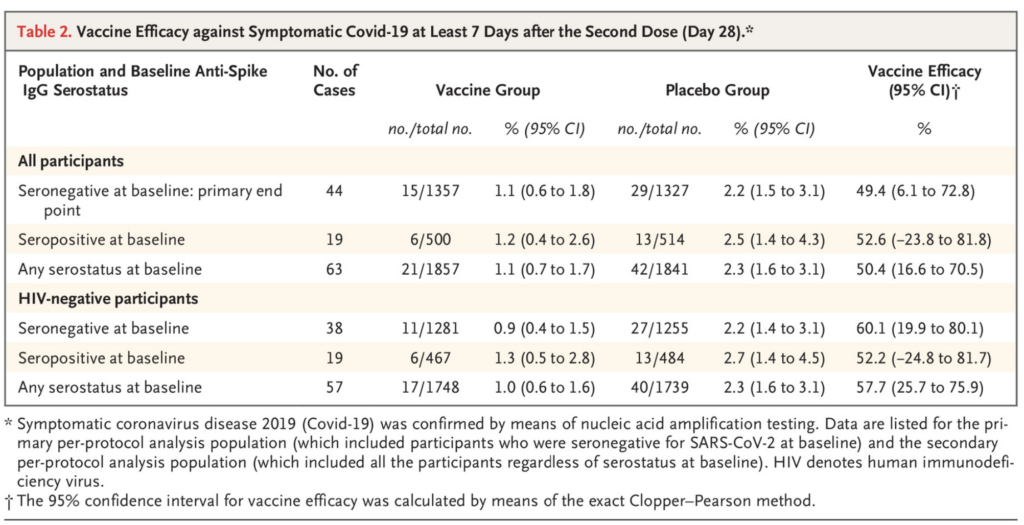
Novavax’s Phase II clinical trial in South Africa showed that the natural immunity of survivors has limited effectiveness against the Beta variant, only 49.4%, which is far lower than the results of the Phase III clinical trial of the vaccine in North America, around 90%. This is most likely to be affected by the immune escape of the Beta variant.
Gamma: the driving force behind the South American epidemic
At the end of 2020, Brazil broke out in the country’s second wave of epidemics, and it also exposed the problem of secondary infections among survivors, from which Scientists discovered the Gamma variant.
Gamma derives new mutations while having same features like Beta, making Gamma likely to have a faster transmission speed and the risk of immune escape at the same time. A Brazilian study supported by the Medical Research Council-So Paulo Research Foundation shows that the Gamma strain spreads 1.7-2.4 times faster in the local area than the non-Gamma strains, and it can also avoid the immune protection brought by 21%-46% of past infections.
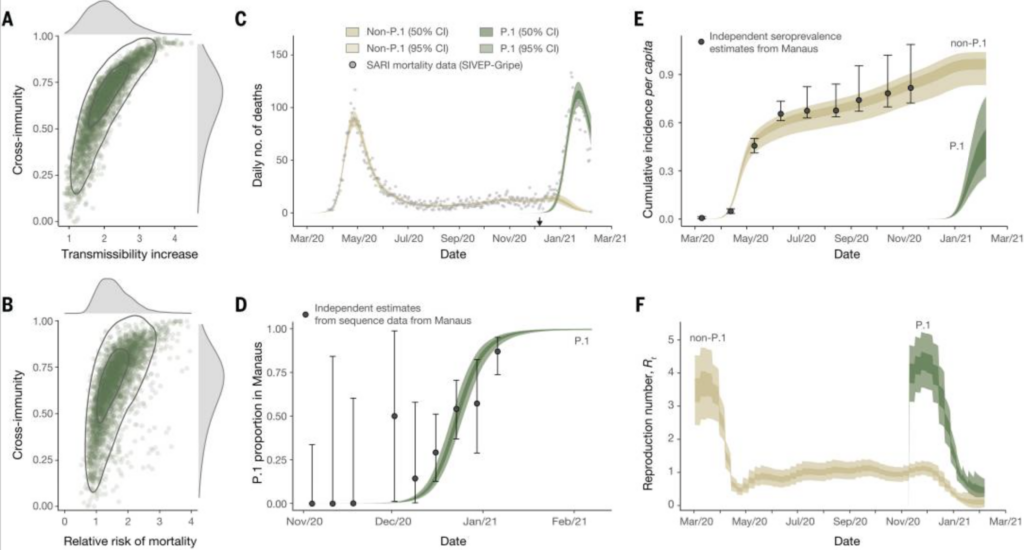
The Gamma variant has also quickly replaced other virus strains in Brazil, becoming the mainstream mutant strain of local infections, and has continued to spread to neighboring countries, becoming the most important coronavirus strain in many countries in South America. Gamma strains are now recorded in 75 countries and regions around the world.
Delta: new variable in the global epidemic
Although Alpha, Beta, and Gamma all have a huge impact on the global epidemic, the biggest shadow of the global COVID-19 pandemic is the Delta variant that has emerged since the outbreak in India in April 2021.
The genetic sequence of Delta was uploaded to the COVID-19 genome sequence database as early as October 2020, so this COVID-19 branch did not only appear when the Indian epidemic broke out in April. However, since the outbreak in India, the Delta mutant strain is spreading globally at an alarming rate, leading to repeated outbreaks in many countries.
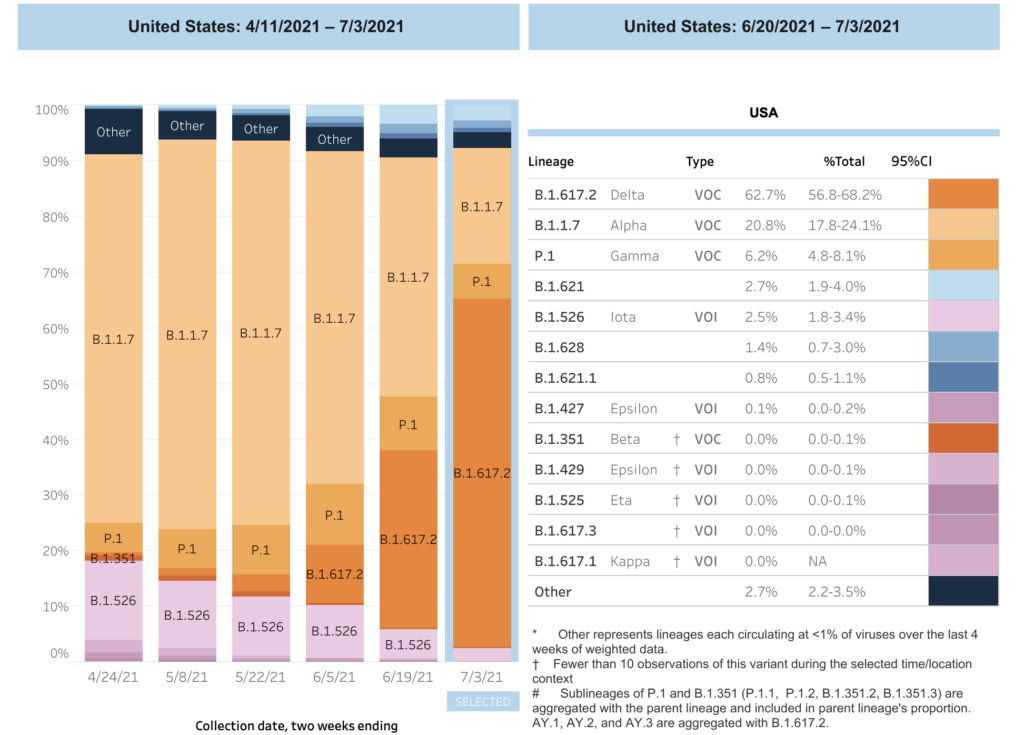
As of 26 July, according to the Weekly Epidemiological Update of the WHO, Delta variant has been recorded in 113 countries and regions around the world. What is even more frightening is that Delta has become the most important mutant strain in many countries within a short period. For example, according to the U.S. Centers for Disease Control and Prevention, Delta has accounted for 62.7% of new cases in the United States, completely replacing the dominant position of the Alpha variant.
According to research published in the Lancet, Delta’s transmission power is 150% higher than that of the Alpha variant, which spreads the fastest before. The R0 may be between 5-8, that is, an infected person can infect 5-8 people and the R0 of the most primitive virus strain of the coronavirus was about 2.5.
Fortunately, although Delta has an impact on the effectiveness of the vaccine, the immune escape observed so far is not serious. According to the latest follow-up study by Public Health England, the effectiveness of the Pfizer/BioNTech vaccine after two doses of the vaccine is 88% against Delta, which is not much lower than the 93.7% of the Alpha variant. Similarly, after two injections of the AstraZeneca vaccine, the effectiveness of Delta is 67%, which is not much different from 74.5% for Alpha. But a very prominent problem is that if only taking one dose, whether it is Pfizer or AstraZeneca, the protective effect is only 30.7%, much lower than the 48.7% for Alpha.
Although the emergence of multiple variants do have a negative impact on the epidemic, the existing vaccines are still effective. According to WHO regulations, if there is a mutation that completely immune escapes, it will be classified as a variant of high consequence. Fortunately, no COVID-19 variant has such serious consequences. And reducing the occurrence of variants through vaccination or public health measures is the key to preventing mutations that cause serious consequences.
(Source: the U.S. Centers for Disease Control and Prevention, the New England Journal of Medicine, AAAS Public Health Emergence Collection)